
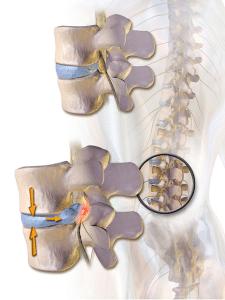
 The basic definition of a herniated disc is a condition whereby portions of a disc, the shock-absorbing cushions between vertebrae are abnormally compressed and protrude outside of the vertebrae. It is widely referred to by as a bulging, ruptured or slipped disc. A disc may move but ‘slipped’ is not medically accurate as the spinal discs are firmly attached between the vertebrae and cannot “slip”. The condition places pressure on the adjacent nerves causing pain, numbness, or weakness either around the damaged disc or anywhere along the area supplied by that nerve. Most herniated discs occur in the lower back (lumbar spine) typically affecting the buttocks, thigh, hips, anal/genital areas, feet and toes. Herniated discs can also occur in the neck (cervical spine) potentially affecting the skull, neck, shoulder, arm and hand.
The basic definition of a herniated disc is a condition whereby portions of a disc, the shock-absorbing cushions between vertebrae are abnormally compressed and protrude outside of the vertebrae. It is widely referred to by as a bulging, ruptured or slipped disc. A disc may move but ‘slipped’ is not medically accurate as the spinal discs are firmly attached between the vertebrae and cannot “slip”. The condition places pressure on the adjacent nerves causing pain, numbness, or weakness either around the damaged disc or anywhere along the area supplied by that nerve. Most herniated discs occur in the lower back (lumbar spine) typically affecting the buttocks, thigh, hips, anal/genital areas, feet and toes. Herniated discs can also occur in the neck (cervical spine) potentially affecting the skull, neck, shoulder, arm and hand.
Symptoms
You can have a herniated disc without knowing it — herniated discs sometimes show up on spinal images of people who have no symptoms of a disc problem. However, most of the patients we treat at the clinic are symptomatic.. The most common signs and symptoms of a lumbar (lower back) herniated disc are:
Arm or leg pain. If your herniated disc is in your lower back, you’ll typically feel the most intense pain in your buttocks, thigh and calf. It may also involve part of the foot. If your herniated disc is in your neck, the pain will typically be most intense in the shoulder and arm. This pain may shoot into your arm or leg when you cough, sneeze or move your spine into certain positions.
- Numbness or tingling. People who have a herniated disc often experience numbness or tingling in the body part served by the affected nerves.
- Muscles served by the affected nerves tend to weaken. This may cause you to stumble, or impair your ability to lift or hold items.
Causes
Some herniated discs are the result of trauma such as a fall or a blow to the back. Others are caused by physically demanding occupations that require repetitive lifting, squatting, prolonged sitting, pulling, pushing, bending and twisting. Additional contributing factors include age related wear of the discs referred to as disc degeneration, increases the risk of a herniation. As you age, your spinal discs lose some of their water content. That makes them less flexible and more prone to rupturing with even a minor strain or twist.
To help prevent a herniated disc-
- Strengthening the trunk muscles helps stabilize and support the spine.
- Maintain good posture. Good posture reduces the pressure on your spine and discs. Keep your back straight and aligned, particularly when sitting for long periods. Lift heavy objects properly, making your legs — not your back — do most of the work.
- Maintain a healthy weight. Excess weight puts more pressure on the spine and discs, making them more susceptible to herniation.
Diagnosis and Treatment
Diagnosis is the most important aspect of determining treatment options for your particular type of herniated disc. As a chiropractor, my diagnostic process includes observation, palpation, a series of orthopedic and neurological tests, postural evaluation, health history and any additional symptoms. Xray and MRI are ordered on a case by case basis. Certain types of hernias can be treated with spinal manipulation, therapeutic exercises, flexion-distraction or pelvic blocking techniques. The specifics of any treatment plan vary based upon pain, level of activity, overall health, and type of hernia. Other types, where the loss of bladder or bowel occur, must be referred to an appropriate specialist. As with any treatment option, don’t hesitate to ask questions about what chiropractic treatments are being recommended and why. You want to make sure you understand what will be done and how it can help relieve your pain.




